Our Commitment to Quality
AultCare's mission is to lead our community to improved health. We are committing to providing you with a superior level of customer service and access to quality care. To achieve our goal, we continually monitor and evaluate our performance against rigorous national and regional standards. To do this, we utilize data from HEDIS® and CAHPS® every year.
What is HEDIS® and CAHPS®?
HEDIS® is the Healthcare Effectiveness Data and Information Set. Insurance companies across the United States participate in HEDIS® data collection making it one of the best ways to gauge our performance against benchmarks. This data set includes over 90 measures that evaluate six different domains, including:
o Effectiveness of Care
o Access/Availability of Care
o Experience of Care
o Utilization and Risk-Adjusted Utilization
o Health Plan Descriptive Information
o Measures Collected Using Electronic Clinical Data System
CAHPS® is the Consumer Assessment of Healthcare Providers and Systems. This set of surveys asks patients to report on their healthcare experiences with both their health plan and their providers. This data is collected annually and plays a key role in how we strive to improve year after year.
UNDERSTANDING THE RESULTS
Below you can find the description and the questions associated with each table listed below.
|
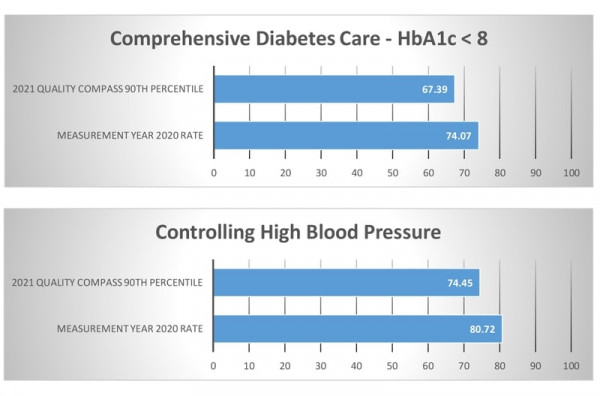
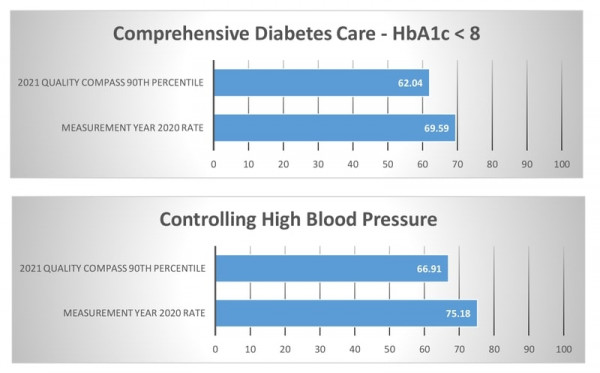
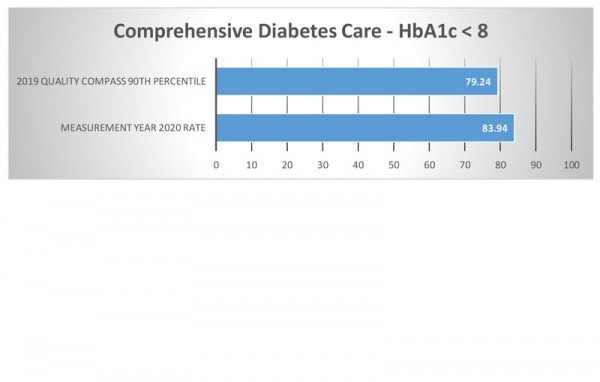
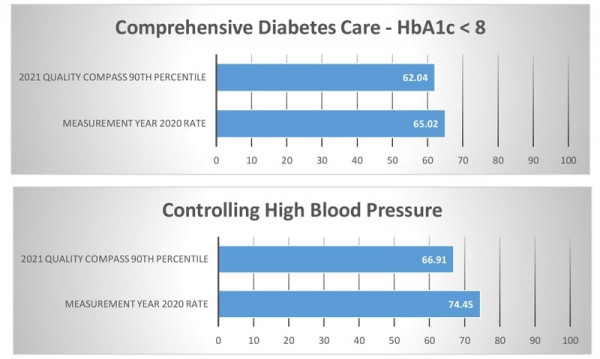
Comprehensive Diabetes Control
The percentage of members ages 18 to 75 years with diabetes who had HbA1c testing.
**The percentage of members ages 18 to 75 years with diabetes who had a nephropathy screening test or evidence of nephropathy (used for QHP data only - HbA1c testing data unavailable). Controlling High Blood Pressure
The percentage of members ages 18 to 85 years who had a diagnosis of hypertension and whose blood pressure was adequately controlled, less than 140/90.
|
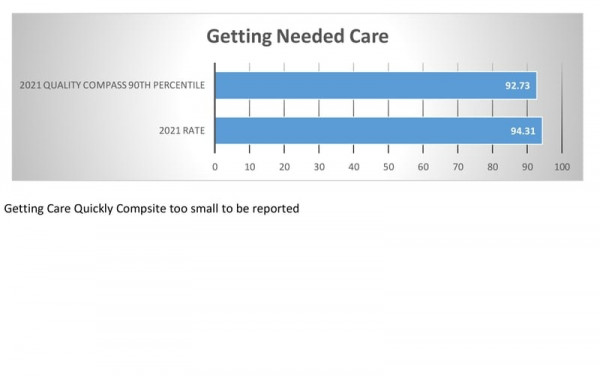
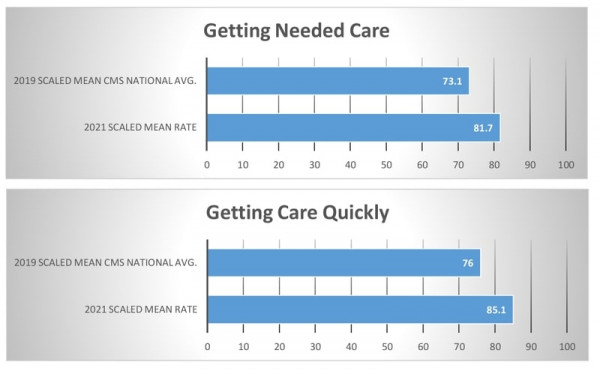
Getting Needed Care
How often was it easy to get the care, tests, or treatment you needed?
How often did you get an appointment to see a specialist as soon as you needed? Getting Care Quickly
When you needed care right away, how often did you get care as soon as you needed?
How often did you get an appointment for a check-up or routine care at a doctor’s office or clinic as soon as you needed? Getting Needed Prescription Drugs
How often was it easy to use your prescription drug plan to get the medicines your doctor prescribed?
How often was it easy to use your prescription drug plan to fill a prescription at your local pharmacy? How often was it easy to use your prescription drug plan to fill a prescription by mail? |
The following HEDIS data represents the measurement year 2020 and reporting the year 2021. The following CAHPS data represents the measurement year 2021.
The Quality Compass benchmarks provided for the below HEDIS® data are representative of the 75th percentile. Please click a chart to review extended information.
How we compare against other plans
HMO
HEDIS® |
CAHPS® |
PPO |
|
HEDIS® |
CAHPS® |
PRIMETIME HEALTH PLAN |
|
HEDIS® |
CAHPS®
|
MARKETPLACE (QHP) |
|
HEDIS® |
CAHPS® |
|
Disclaimers:
The source for certain health plan measure rates and benchmark (averages and percentiles) data ("the Data") is Quality Compass 2021 and is used with the permission of the National Committee for Quality Assurance ("NCQA"). Any analysis, interpretation, or conclusion based on the Data is solely that of the authors, and NCQA specifically disclaims responsibility for any such analysis, interpretation or conclusion. Quality Compass is a registered trademark of NCQA. The Data comprises audited performance rates and associated benchmarks for Healthcare Effectiveness Data Information Set measures ("HEDIS") and HEDIS CAHPS survey measure results. HEDIS measures and specifications were developed by and are owned by NCQA. HEDIS measures and specifications are not clinical guidelines and do not establish standards of medical care. NCQA makes no representation, warranties or endorsement about the quality of any organization or clinician who uses or reports performance measures, or any data or rates calculated using HEDIS measures and specifications, and NCQA has no liability to anyone who relies on such measures or specifications. NCQA holds copyright in Quality Compass and the Data and may rescind or alter the Data at any time. The Data may not be modified by anyone other than NCQA. Anyone desiring to use or reproduce the Data without modification for an internal, noncommercial purpose may do so without obtaining approval from NCQA. All other uses, including commercial use and/or external reproduction, distribution, or publication, must be approved by NCQA and are subject to a license at the discretion of NCQA 2021 National Committee for Quality Assurance, all rights reserved. CAHPS is a registered trademark of the Agency for Healthcare Research and Quality (AHRQ). HEDIS® is a registered trademark of the National Committee for Quality Assurance (NCQA). We have listed websites here to help you find out more about health care quality. This information is provided only as a service to readers and does not imply endorsement or promotion of these organizations, any products or services they offer, or any groups they may link with through their websites. |
Related LinksAgency for Health Care Research and Quality Tool to review National Scorecards to make health care safer and improve quality.
Hospital Compare Tool to provide you information on hospitals in your area that have submitted quality information for Hospital Comparisons.
|